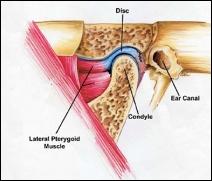
The temporomandibular joint (TMJ) is a small joint located in front of the ear where the skull and lower jaw meet. The pair of TMJs allows the lower jaw to move and function.
Anatomy of the TMJ
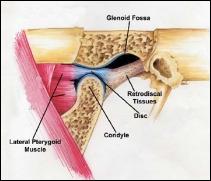
The jaw joint is unique because it has not only has a hinge motion but also a forward sliding motion. There is a cartilage-like disc that acts as a cushion to absorb stress and allows the head (called the condyle) of the mandible (the lower jaw) to move easily within the socket as the mouth opens and closes.
Temporomandibular joint disorders are fairly common, especially in adult females, and have a variety of symptoms. Patients may notice chewing pain, difficulty opening the mouth, earaches, headaches, or pain in front of the ear or on the sides of the face. There may also be clicking, popping, or grating sounds in the joint. There is often a history of some sort of trauma or injury to the joint, but not always.

Possible Causes for TMJ Disorders
Determining the cause of a TMJ problem is critically important. The three broad categories of TMJ disorders are spasm of the jaw muscles, problems with the actual jaw joint structures, and chronic neurologic pain. Many patients have a combination of these problems. A careful history, thorough exam, and computerized imaging will help Dr. Stout arrive at the correct diagnosis.
Muscle Problems: Muscle pain usually is felt on the entire side of the lower face, and may even extend up toward the ears, temples and side of the scalp. TMJ muscle pain often worsens after chewing. The actual jaw muscles are usually painful to touch, and the jaws may not open as wide due to pain. Chronic jaw muscle spasm is usually caused by chronic overuse such as clenching or grinding of the teeth, gum chewing, or habits such as cheek biting or nail biting. Stress or even cold weather can also cause acute or chronic muscle spasm. Missing posterior teeth also place an excessive burden on the jaw muscles and joints and can contribute greatly to TMJ disorders. This is one of the reasons replacing missing back teeth is so important, even if they are not seen by others.
Temporomandibular joint inflammation may be caused by osteoarthritis, the typical “wear and tear” degeneration that can affect any joint in the body. It may also be an extension of an autoimmune condition such as rheumatoid arthritis. Joint inflammation causes progressive limitation of motion, changes in the fit or occlusion of your teeth, and grating sounds as the smooth joint surface degenerates.
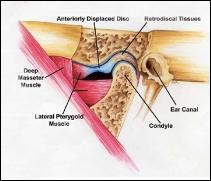
Another type of joint problem involves dislocation of the disc between the jawbone condyle and the socket. A displaced disc may produce clicking or popping sounds, limit jaw movement, and cause pain when opening and closing the mouth. After a time, the disc can become permanently deformed or even develop a perforation. Chronic disc problems can lead to degenerative arthritis of the joint.
Neurologic Pain Disorders: Some neurologic pain disorders mimic TMJ disorders because the pain is felt in the area of the jaws, teeth, or joints. These pain disorders are caused by nerve inflammation unrelated to the teeth or jaws. After other causes have been eliminated, a neurologic disorder might be considered and appropriate treatment using medicines might be appropriate.
Treatments for TMJ Disorders
Conservative, non-surgical treatment is usually the starting point for all TMJ disorders. This may include a non-chewing diet, anti-inflammatory medications, and stopping the offending habits such as gum chewing, nail-biting, chewing hard foods or opening widely. It may also be appropriate to administer bite plate (orthotic splint) therapy. If non-surgical treatment is unsuccessful or if there is clear joint damage, surgery may be indicated.
Surgical treatment usually involves arthrocentesis, a minimally-invasive procedure done under sedation in our office. Access is created into the joint and fluids are drained off and replaced with anti-inflammatory steroid medication. Your joint function and range of motion can also be evaluated and improved while you are completely asleep. For more severe cases, arthroscopy can repair damaged tissue by a direct surgical approach. It is rare that more significant joint reconstruction is needed.